Understanding California Education Code §56332:
A Guide for Schools and Families
California’s SB1016 has become EC56332. Now what?
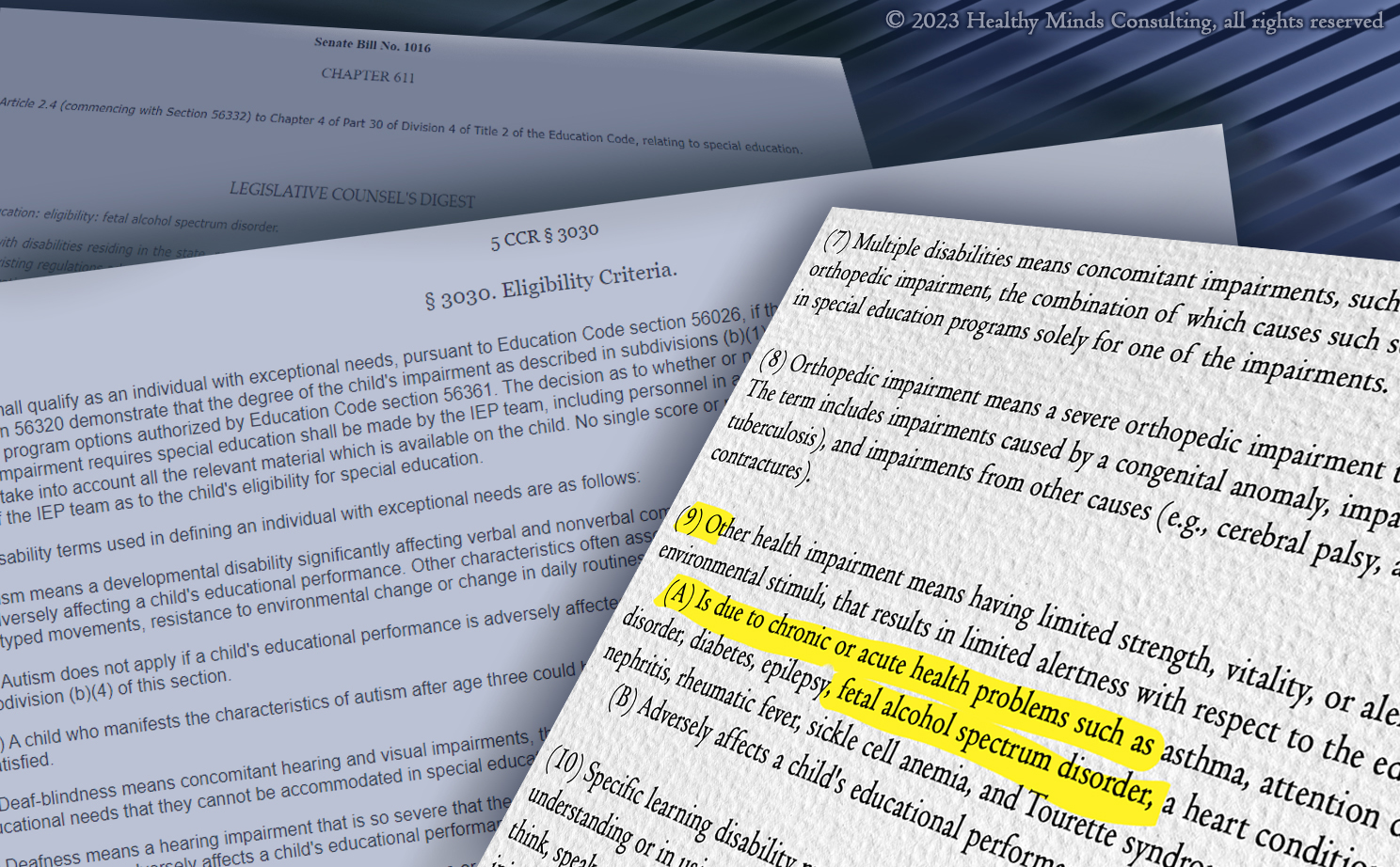
On January 1st, 2023, California’s Senate Bill 1016 became CA Education Code §56332. This law includes Fetal Alcohol Spectrum Disorders (FASD) as a named condition under the special education eligibility category of Other Health Impairment (OHI). Why is this important? And what does it mean for students, families and educators now that the law is in place? We will explore the answers to these questions and more, below.
What is FASD and why does it matter if it is listed explicitly under a specific IEP eligibility category?
Fetal Alcohol Spectrum Disorders occur when a child is exposed to alcohol during prenatal development. Alcohol is a teratogen, meaning it is harmful to human development. When alcohol is consumed by someone who is pregnant, the embryo or fetus is exposed to the alcohol as well. 1 The alcohol impacts the baby’s nervous system development, which includes the brain, and often impacts additional areas of the body depending on when the alcohol was consumed and how much alcohol was consumed at any given point. 2
Students who are struggling in school or who are having difficulty accessing their education should be assessed to determine the need for an Individualized Education Program (IEP). 3 In order to qualify for an IEP under the Individuals with Disabilities Education Improvement Act* (IDEIA, typically referred to simply as IDEA), students must be identified as having a disability that falls into one of 13 eligibility categories (some states have created additional eligibility categories) and need special education and related services in order to access their educational program. 4
Current estimates are that 1 in 20 school age children in the United States have FASD.
While FASD has been around as long as humans have consumed alcohol, the term Fetal Alcohol Syndrome was only formally introduced by the medical community in 1973 and the understanding of the entire spectrum of FASD came into understanding in the 1990s and was formally adopted in 2004. 5 Current estimates are that 5% (1 in 20) of school age children in the United States have FASD. 6 Despite the historical presence and the prevalence of FASD, there is still a lot of misinformation and misunderstanding about this disability. Most families and professionals are unaware of the spectrum of symptoms that may be present or the types of interventions that are effective or ineffective with this population. Because most people lack a detailed understanding of this disability, it often goes unrecognized, unidentified, and unaddressed. 7-11 Much of the time, the presenting symptoms of someone with FASD overlap other psychiatric, psychological, or medical conditions and are therefore misidentified 9 as another disability altogether. The challenge with misidentification is that disabilities with different etiologies often respond to various treatments differently. There is no one-size-fits-all treatment for all disabilities (nor does every disability need treatment or interventions). Each unique situation must be understood both in context of what is known (we are talking facts and educated hypotheses here, not inaccuracies – no matter how socially accepted they are) and what is unique to that individual.
When it comes to IEPs, students with FASD are typically misidentified as having a different disability, or even assumed to be socially maladjusted, and either receive inappropriate or insufficient supports and services at school. I firmly believe this is not due to any malintent by educators, but rather a naiveté about this disability that can be rectified by training in the educational strategies that are most helpful for students with FASD. Without knowledge of which supports and services might be most appropriate, or those that may be contraindicated, students continue to struggle and their educational needs often increase. Many times students receive services under LD, OHI, SLI, or ID eligibility categories in elementary school. However, because these students’ true underlying area of disability was not accurately identified or addressed, behavioral challenges tend to rise and many, if not most, students with FASD have an ED eligibility by the time they reach middle school or high school. While IDEA states that services are not tied to eligibility categories, the reality is that many schools and educational programs have regulations impacting which students they accept or serve and many of those regulations are tied to eligibility categories.
All of this is exacerbated by stigma. Our society still tends to blame parents for drinking during pregnancy and for their children’s behavioral challenges. Many parents are not comfortable disclosing that they consumed alcohol during their child’s prenatal development which further compounds the difficulty of obtaining accurate identification of the disability as well as impacting the chance of receiving effective services and supports.
By including FASD as a named condition under the OHI eligibility category, it helps to clarify the health-related nature of this disability and brings attention back to the brain-based (and physiologic) nature of FASD. Accurate eligibility in an IEP is often the first step toward appropriate supports and services.
Wasn’t FASD always supposed to be identified under OHI?
The simple answer is yes. During the reauthorization of IDEA (changing it to IDEIA) in 2004, the federal government responded to comments from the public on the new changes (and those the public recommended be made). The federal regulations discuss FAS† and the public’s desire to have it listed explicitly under OHI. The committee making decisions at the time, felt that FAS† obviously fell under OHI and there was no need to specify it directly. Unfortunately, their assumption has not proven to be accurate with regard to students’ experiences and therefore many states are moving to rectify this by naming FASD specifically under the OHI eligibility category.
Now that FASD is listed under OHI in California, what changes can schools and families expect?
 The group that advocated for this new law, FASDNow!, is rolling out trainings for educators, service providers, families, and anyone else who attends IEP meetings for students with FASD. California SELPA (Special Education Local Plan Area) leaders received an initial training in early July, 2023, and FASDNow! is collaborating with local educational agencies (LEA) throughout the state to ensure that every educational entity that wants training in FASD receives it. The more knowledgeable educators and service providers are in understanding and identifying FASD, as well as ensuring students receive appropriate and effective supports and services, the more likely we are to reduce drop-out rates and juvenile justice involvement for this population.
The group that advocated for this new law, FASDNow!, is rolling out trainings for educators, service providers, families, and anyone else who attends IEP meetings for students with FASD. California SELPA (Special Education Local Plan Area) leaders received an initial training in early July, 2023, and FASDNow! is collaborating with local educational agencies (LEA) throughout the state to ensure that every educational entity that wants training in FASD receives it. The more knowledgeable educators and service providers are in understanding and identifying FASD, as well as ensuring students receive appropriate and effective supports and services, the more likely we are to reduce drop-out rates and juvenile justice involvement for this population.
While symptoms of FASD tend to increase as children age, identifying FASD early on is a protective factor and reduces the likelihood of secondary disabilities.15,16 By providing FASD-informed interventions and supports, schools have an inimitable opportunity to contribute to the well-being of students experiencing FASD. The passing of SB1016 in California is creating increased awareness of this disability and potentiality for increasing appropriate supports and services for students. Educators who are knowledgeable of the common symptoms of FASD and who have training in brain-based neurobehavioral approaches will find themselves more effective with supporting their students when behavioral challenges or variability in cognitive output occur.
For families that are aware of their child’s diagnosis but not receiving services specific to FASD and are interested in redesignation under OHI, or new assessments with reconsideration of FASD specifically, the coming year may be a good time for reconsideration of eligibility. Families can write a letter to their child’s school requesting reassessment. It is helpful to include all areas of suspected need when requesting new assessments. The more thorough families can be in describing their child’s specific needs and challenges, the more it will help the school identify which assessments may be appropriate and which service providers many need to be involved in completing the assessments. We have included a sample letter you can download here.
For students who may not yet be identified by their families or schools, I encourage you (families, educators, service providers, and anyone who supports the child in any way) to learn more about FASD. With a prevalence of one in twenty school age children having FASD6, if the knowledge does not apply directly to you or your child or student, it is likely to be helpful in better understanding, and hopefully being more empathetic with, someone you know or interact with.
Assessors (school psychologists, speech and language pathologists, occupational therapists, and anyone else completing assessments for students) who participate in the FASDNow! training series will learn how to identify red flags that signify when FASD should be considered. They will learn about the many different areas of suspected need that are often associated with prenatal alcohol exposure and which intervention strategies and supports are most likely to be beneficial, as well as which are likely to be ineffective or possibly cause harm or an exacerbation of symptoms. Once trained, assessors will be able to identify students who may have FASD or who may benefit from FASD-informed approaches. Using this knowledge to tailor IEP services to both the suspected (or known) area of disability and the individualized needs of the specific student will greatly enhance the efficacy of the services and supports provided.
For families that have been trying to access services for their child with FASD but have had difficulty doing so, we have created a sample letter requesting an initial assessment that can be downloaded here. I am hopeful that the rollout of education about FASD that will be occurring in California will create a supportive environment to restate your concerns and your child’s needs. I believe as we expand education on FASD throughout California schools, FASD will one day be a well understood area of disability and students will receive supportive and effective services and accommodations from school professionals with knowledge and understanding of this distinctive disability.
Looking to the future
Training all the educators in all the schools in California is a daunting task and it will take a considerable amount of time. Many SELPAs, schools, districts, and individuals have already noted interest in becoming trained on FASD and as more learn about EC §56332 there will undoubtedly be an increased need for training. While quality training is essential, you do not have to wait for training to start supporting students who may have FASD. Steps can be taken both before and during the training roll-out to facilitate positive educational situations for students.
In order to support the journey toward supportive educational environments for students who have experienced prenatal alcohol exposure, I have included action items that can be implemented now and are aligned with best practices in working with students with FASD.
- Collaborate with families and education professionals. The more we can learn from one another about the unique needs of each individual with FASD, the more effective we can be at creating supportive learning environments.
- Utilize Universal Design for Learning (UDL) principles to enhance learning opportunities. UDL will support the educational needs of students with FASD (as well as all other learners in the class).
- Seek out brain-based teaching methodologies. Delving into current neuroscience research will illuminate how we are reconfiguring our societal understanding of behaviors.
- Look deeper. When trying to understand what is going on for a student, look for the underlying need that the student is trying to meet. Try to identify the deeper source that underlies traditional views of positive behavioral interventions and gets to the root of the challenge.
- Think outside the box. Many aspects of FASD are contrary to people’s expectations (one of the reasons these students are often unidentified or misidentified) and require paradigm shifts in order to effectively address the presenting challenges. By thinking creatively, we can often find supportive practices that will have positive outcomes.
- Get consultation from professionals in the field. Reaching out to those with specific knowledge about FASD within the delineated area you want to explore (assessments, IEPs, interventions, etc.) will provide you with guidance and direction while awaiting more in-depth training and can also be a boon to your skills after receiving training and when working to implement new or different tools.
- Begin identifying Red Flags for FASD by utilizing this tool from FASDNow! While a flyer is no substitute for in-depth training, it can definitely get you thinking about situations and students you work with and when it might be worthwhile to consider FASD as a contributing factor.
- Start with accommodations. When you are working with a student who is struggling in an area of their education, consider which accommodations may be able to be implemented to better support their learning. What is needed for this student to effectively access their curriculum? What changes can we make to the classroom, playground, or school environment that will enable the student to participate more effectively?
- Implement strength-based approaches and create strength-based IEPs. Discovering a student’s strengths and incorporating those strengths into their IEP goals will enhance their ability to meet the goals.
- Approach every child with empathy. Coming to challenges with a mindset and heartset of empathy for what the student may be experiencing changes the way we respond. Students have full lives that encompass many experiences unknown to those educating them and often unknown to their families as well. The more we approach all beings with empathy, the more likely we are to open to new and helpful ways of viewing needs.
Having FASD listed explicitly under the OHI category is a helpful step toward accurate identification of needs and facilitation of effective support and strategies, but it is just the tip of the iceberg. The more we can collectively embrace the need to learn about this unique and prevalent disability, the better chance we have of nurturing students with FASD throughout their educational careers and into their adult lives.
*In 2004, Congress reauthorized IDEA as the Individuals with Disabilities Education Improvement Act (IDEIA); however, it continues to be commonly referred to as IDEA.
†Fetal Alcohol Syndrome (FAS) was more commonly known and information about this disability (one of the diagnoses under the Fetal Alcohol Spectrum Disorders label) has been taught to professionals with more regularity over the past few decades. However, we have since learned that FAS (which includes specific facial features associated with prenatal exposure to alcohol at a very specific time in early embryonic development) only constitutes approximately 10% of those negatively impacted by prenatal alcohol exposure12. The brain-based neurological component of prenatal alcohol exposure is something that is impacted throughout prenatal development and therefore has many different presentations depending on the amount and timing of alcohol exposure13. Because of this knowledge, the term Fetal Alcohol Spectrum Disorders (FASD) has been coined to address all of the various diagnoses related to prenatal alcohol exposure5.
 Kelly Rain Collin, Ed.M. is founder and director of Healthy Minds Consulting. Kelly Rain has been working with at-risk children and youth since 1990, including children who are deaf or hard of hearing, children living with HIV/AIDS, and children prenatally exposed to alcohol and other drugs. She has provided educational consultation and advocacy support to therapists and families for more than twenty years. Kelly Rain conducts specialty consultation and trainings for schools, advocates, attorneys, families, and other professionals on the interface between FASD (Fetal Alcohol Spectrum Disorders) and the IEP, how to improve IEP goal writing by going Beyond SMART Goals, and other related topics. She also hosts the FASD & the IEP Mentorship Coalition, a monthly gathering for anyone who participates in IEPs and wants to dive deeper into how to structure IEPs and supports in ways that will allow students with FASD to thrive.
Kelly Rain Collin, Ed.M. is founder and director of Healthy Minds Consulting. Kelly Rain has been working with at-risk children and youth since 1990, including children who are deaf or hard of hearing, children living with HIV/AIDS, and children prenatally exposed to alcohol and other drugs. She has provided educational consultation and advocacy support to therapists and families for more than twenty years. Kelly Rain conducts specialty consultation and trainings for schools, advocates, attorneys, families, and other professionals on the interface between FASD (Fetal Alcohol Spectrum Disorders) and the IEP, how to improve IEP goal writing by going Beyond SMART Goals, and other related topics. She also hosts the FASD & the IEP Mentorship Coalition, a monthly gathering for anyone who participates in IEPs and wants to dive deeper into how to structure IEPs and supports in ways that will allow students with FASD to thrive.
Related article: FASD and the Need for Early and Effective Interventions
References:
1 Centers for Disease Control and Prevention. (2022, November 4). Fetal Alcohol Spectrum Disorders (FASDs).
https://www.cdc.gov/ncbddd/fasd/facts.html#:~:text=Table%20of%20Contents,a%20mix%20of%20these%20problems
2 The Alcohol Pharmacology Education Partnership. (n.d.). Module 5: Alcohol and Babies?!? » Content: When Can Alcohol Damage the Fetus?. Retrieved July 30, 2023 from
https://sites.duke.edu/apep/module-5-alcohol-and-babies/content-when-can-alcohol-damage-the-fetus/
3 IDEA Individuals with Disabilities Education Act. (2017, May 3). Sec. 300.111 Child find.
https://sites.ed.gov/idea/regs/b/b/300.111
4 IDEA Individuals with Disabilities Education Act. (2017, May 3). Sec. 300.8 Child with a disability.
https://sites.ed.gov/idea/regs/b/a/300.8
5 Janet F. Williams, Vincent C. Smith, the COMMITTEE ON SUBSTANCE ABUSE; Fetal Alcohol Spectrum Disorders. Pediatrics November 2015; 136 (5): e20153113. 10.1542/peds.2015-3113
https://publications.aap.org/pediatrics/article/136/5/e20153113/33770/Fetal-Alcohol-Spectrum-Disorders?autologincheck=redirected
6 May PA, Chambers CD, Kalberg WO, et al. Prevalence of Fetal Alcohol Spectrum Disorders in 4 US Communities. JAMA. 2018;319(5):474–482. doi:10.1001/jama.2017.21896
https://jamanetwork.com/journals/jama/fullarticle/2671465
7 Petrenko, C. L., Tahir, N., Mahoney, E. C., & Chin, N. P. (2014). Prevention of secondary conditions in fetal alcohol spectrum disorders: identification of systems-level barriers. Maternal and child health journal, 18(6), 1496–1505.
https://doi.org/10.1007/s10995-013-1390-y
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4007413/
8 May, P. A., Baete, A., Russo, J., Elliott, A. J., Blankenship, J., Kalberg, W. O., Buckley, D., Brooks, M., Hasken, J., Abdul-Rahman, O., Adam, M. P., Robinson, L. K., Manning, M., & Hoyme, H. E. (2014). Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics, 134(5), 855–866.
https://doi.org/10.1542/peds.2013-3319
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4210790/
9 Ira J. Chasnoff, Anne M. Wells, Lauren King; Misdiagnosis and Missed Diagnoses in Foster and Adopted Children With Prenatal Alcohol Exposure. Pediatrics February 2015; 135 (2): 264–270. 10.1542/peds.2014-2171
https://publications.aap.org/pediatrics/article-abstract/135/2/264/33477/Misdiagnosis-and-Missed-Diagnoses-in-Foster-and [Abstract]
10 O Connor, M. J., McCracken, J. T., & Best, A. (2006). Under recognition of prenatal alcohol exposure in a child inpatient psychiatric setting. Mental Health Aspects of Developmental Disabilities, 9(4), 105.
https://www.semel.ucla.edu/sites/default/files/publications/Under%20Recognition%20of%20Prenatal%20Alcohol%20Exposure_0.pdf
11 Elias, E. (2013). Improving Awareness and Treatment of Children With Fetal Alcohol Spectrum Disorders and Co-occurring Psychiatric Disorders. Note from the editors, 71.
https://lcfasd.com/wp-content/uploads/2017/09/FASD-MENTAL-HEALTH.pdf
12 Andrew, G. (2010). Diagnosis of FASD: An Overview. In Fetal Alcohol Spectrum Disorder (eds E.P. Riley, S. Clarren, J. Weinberg and E. Jonsson).
https://doi.org/10.1002/9783527632510.ch7
13 Riley EP, McGee CL. Fetal alcohol spectrum disorders: an overview with emphasis on changes in brain and behavior. Exp Biol Med (Maywood). 2005 Jun;230(6):357-65. doi: 10.1177/15353702-0323006-03. PMID: 15956765.
https://pubmed.ncbi.nlm.nih.gov/15956765/ [ABSTRACT]
14 Streissguth, A. P., Bookstein, F. L., Barr, H. M., Sampson, P. D., O’Malley, K., & Young, J. K. (2004). Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. Journal of developmental and behavioral pediatrics : JDBP, 25(4), 228–238.
https://doi.org/10.1097/00004703-200408000-00002 [ABSTRACT]
15 Carmen Rasmussen, PhD and others, Neurobehavioural outcomes of children with fetal alcohol spectrum disorders: A Canadian perspective, Paediatrics & Child Health, Volume 13, Issue 3, March 2008, Pages 185–191,
https://doi.org/10.1093/pch/13.3.185
https://academic.oup.com/pch/article/13/3/185/2648057
16 Streissguth, A. P., Barr, H. M., Kogan, J., & Bookstein, F. L. (1996). Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE). Final report to the Centers for Disease Control and Prevention (CDC), 96-06.
http://lib.adai.uw.edu/pubs/bk2698.pdf